Ref: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3134027/
Summary:
- Infected tibia wound and knee joint after surgery.
- Ischemic wounds not healing after 15 days of antibiotics.
- Amputation was advised by medical doctor.
- Topical ozone O3 twice daily + O3 autohemotherapy once daily.
- Both bone and soft tissue healed withiout complications.
- No amputation was needed after successful ozone O3 treatment.
|
Prasham Shah, Ashok K Shyam,1 and Sambhav Shah
Department of Orthopaedics, Leelavati Hospital, and Saifee Hospital, Mumbai, India
1Indian Orthopaedic Research Group, Thane, and Sancheti Institute for Orthopaedics and Rehabilitation, Pune, India
Address for correspondence: Dr. Ashok K. Shyam, Sancheti Institute of Orthopaedics and Rehabilitation, 16 Shivaji Nagar, Pune 411 005, Maharashtra, India. E-mail: drashokshyam@yahoo.co.uk
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
________________________________________ |
Adjuvant Combined O3 Ozone Therapy for Extensive Wound Over Tibia
Abstract:
- Disinfectant and antibacterial properties of ozone are utilized in the treatment of nonhealing or ischemic wounds. We present here a case of 59 years old woman with compartment syndrome following surgical treatment of stress fracture of proximal tibia with extensively infected wound and exposed tibia to about 4/5 of its extent.
- The knee joint was also infected with active pus draining from a medial wound. At presentation the patient had already taken treatment for 15 days in the form of repeated wound debridements and parenteral antibiotics, which failed to heal the wound and she was advised amputation.
- Topical O3 ozone therapy twice daily and O3 ozone autohemotherapy once daily were given to the patient along with daily dressings and parenteral antibiotics.
- Within 5 days, the wound was healthy enough for spilt thickness skin graft to provide biological dressing to the exposed tibia bone. Topical ozone therapy was continued for further 5 days till the knee wound healed.
- On the 15th day, implant removal, intramedullary nailing, and latissimus dorsi pedicle flap were performed.
- Both the bone and the soft tissue healed without further complications and at 20 months follow-up, the patient was walking independently with minimal disability.
________________________________________ |
Introduction
Ozone is well established as a powerful disinfectant and is considered as one of the best agents to sterilize water.1,2 The antibacterial properties of ozone have been studied in detail and have been extensively reported in dental and other literature.
3–6 Calderon and Kaufman7 treated (n=63) these cases with topical ozone therapy and reported complete healing of ulcers in 49 patients. In the remaining 14 patients, the bacterial growth was controlled by ozone therapy. De Monte et al. reported 2 cases of leg ulcers treated by ozone autohemotherapy (AHT) with healing achieved in both the cases.
8 Bocci recommended the combined use of topical and AHT stating that a synergistic effect would lead to rapid healing of the wounds.3 Here we present a case of compartment syndrome following surgical treatment of stress fracture of proximal tibia with extensively infected wound and exposed tibia to about 4/5 of its extent. Adjuvant combined ozone therapy was used in this patient with good results.
________________________________________ |
Case Reports
A 59-year-old woman had a minor fall with injury to the right leg. She was diagnosed as having stress fracture of the proximal tibia [Figure 1a] and a plaster cast was applied above the knee at a different institution. She was evaluated 1 month later with no evidence of union.
Figure 1.
(a) Radiograph showing stress fracture of proximal tibia; (b) Dual plating using two incisions as the fracture did not show any signs of healing with 1 month of plaster cast.
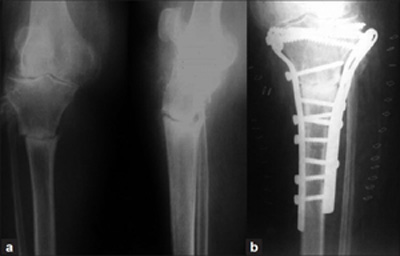
The patient underwent surgery in the form of dual plating [Figure 1b]. On the 3rd day postoperative, compartment syndrome was diagnosed. During fasicotomy, necrosis of the entire anterior compartment was noted and tibialis anterior and a part of the peroneus musculature were debrided and excised. The fasicotomy wound got infected with the spread of infection to the knee joint, which drained through a large wound on the medial side.
Wound cleaning and repeated debridements were performed for 2 weeks with parenteral antibiotics with no improvement in the status of the wound. Finally, the patient was advised amputation.
The patient did not consent for amputation and came to our center for further management. At the time of presentation, the wound was covered with necrotic tissue and slough and middle 4/5 of the tibia bone exposed with blackening at the lower end [Figure 2a].
Figure 2.
(a) Clinical appearance of the wound at the time of presentation showing necrotic tissue and exposed bone and draining wound communicating to the knee joint (arrow); (b) Limb being exposed to topical ozone therapy; (c) Split thickness skin graft on the wound.
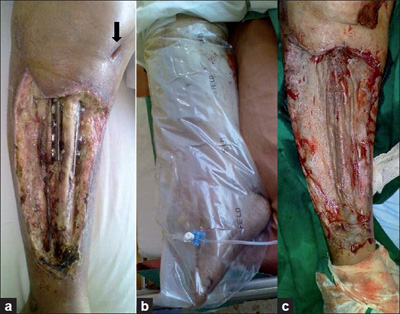
Active pus was discharging from the knee joint through the medial wound [Figure 2a]. The knee joint had painful movements of only 10°–30°, whereas the ankle had 20° of equinus deformity. The patient was a known case of hypertension and was on medication since last 8 years. There was no history of diabetes or any other medical or surgical illness.
Biochemical investigations showed hemoglobin of 10.2 mg% with rest of the parameters within normal limits. A swab from the wound cultured Staphylococcus aureus. The patient was taken in for the first debridement. Three holes were drilled in the tibia to verify bone viability. All the 3 sites had active bleeding from the bone. A thorough debridement of the wound was done with removal of all the dead and necrotic tissue.
Postsurgery the entire lower leg was wetted with sterile distilled water and covered with a sterile plastic bag, which has outlet and inlet valves. First, air was sucked out of the bag and then ozone mixture at a dose of 70 μg was infused into the bag till the bag was full with the gas. After the entire dose was infused, the ozone machine was switched off and the bag was left in place for the next 30 min [Figure 2b]. These sittings were given 2 times a day.
Antibiotics in the form of ceftriaxone 1 g and amikacin 500 mg twice daily and metronidazole 100 mL thrice daily were given. Autohemotransfusion of ozone was done once daily by taking out 50 cc of the patient's blood and ozonizing it with 70 μg of ozone and then re-injecting it into the patient.2 Routine wound cleaning and dressing were performed daily. This protocol was followed for the next 4 days.
On day 5, the wound was granulating and red with minimal necrosed tissue; however, the knee wound was still having some slough. A decision to provide biological cover to the exposed tibia bone was taken and a split thickness skin grafting was done on 5th day postadmission [Figure 2c].
Postoperatively, further 5 sittings of local ozone were given till the knee wound became healthy and started granulating at the base. The tibia skin graft healed well with no signs of graft rejection. At this time, the knee wound had healthy granulation tissue. The skin graft was well accepted over the surrounding soft tissues, the graft over the bone and implant was removed on the 15th day from admission and the tibia was fixed with intramedullary interlocked nail and a latissimus dorsi pedicle flap [Figure 3].
Figure 3.
(a) Latissimus dorsi pedicle flap was done to cover the wound and implant removal and intramedullary nailing was performed in a single stage.

The flap was taken up well and the knee wound healed by secondary intention. Knee and ankle mobilization were started on the 3rd day postsurgery. The follow-up examination had the flap healing well and bone showing progressive signs of union. No further reactivation of infection was noted.
The bone healed in 4 months with the patient starting to walk toe-touch weight bearing by 2 months, partial weight bearing 4 months, and full weight bearing 6 months. At 20 months followup the patient is walking full weight bearing and using an anti–foot-drop splint. The knee has a range of movement of 10°–100° [Figure 4]. The patient is able to perform her daily activities and is able to walk 200 m distance at a stretch.
Figure 4.
(a) Clinical and radiographic appearance at 20 months postsurgery showing healing of both soft tissue and the bone.

________________________________________ |
Discussion
Ozone therapy is a recognized treatment modality in more than 16 countries with more than 35 years of clinical experience, yet a widespread use is still limited.9,10 Ozone therapy has been shown both to improve wound healing, modulate immune system, and act as an antibacterial agent.11 In our case, the nonhealing and necrotic wound seen postcompartment syndrome may be associated with continued tissue ischemia, reperfusion injury, and imbalanced tissue homeostasis and microcirculation.
12 In blood, ozone almost immediately disintegrates forming reactive oxygen species and lipid oxidation products.3,11 The lipid oxidation products cause vasodilatation by acting on the endothelium, causing release of prostacyclin, interleukin-8, and nitric oxide.
2,3,13–15 Reactive oxygen species cause platelet aggregation and release of platelet-derived growth factors, transforming growth factor β, and interleukin-8, which play a major role in rapid wound healing.
16 Ozone AHT is also shown to improve the hemorrheologic properties and increase the oxygen delivery to the more ischemic tissues.3,17 The therapeutic oxidative stress caused by the AHT also leads to upregulation of the intracellular antioxidant enzymes and production of heme oxygenase-1 and heat-stable protein-70, which help in protecting the tissues from ischemia/reperfusion and inflammation and also play a role in wound healing.
3,11,18–20 In our case, the patient was 59 years old and immunosenescence may also be a cause of impaired wound healing.21 Ozone AHT induces release of cytokines, such as TNF-α and interleukins, which activate the neutrophils and lymphocytes.3,11,22,23 These reinfused ozonated lymphocytes further activate other cells in a paracrine manner, causing widespread immune stimulation.
3,11 Although ozone has excellent bactericidal, virucidal, and also antiprotozoal properties, this action is nullified by the presence of endogenous antioxidant in the plasma, making ozone ineffective in sterilizing blood.3,24 This is a major reason to combine the AHT with topical ozone therapy. We soaked the wound with distilled water and infused ozone in a sealed bag. Ozone readily dissolves in water and acts as a cleansing solution and powerful disinfectant. It is bactericidal to most antibiotic-resistant bacteria, including methicillin-resistant S. aureus and anaerobes.
527,40 Oxidative injury is a potential complication of ozone therapy; and in blood, ozone leads to the formation of reactive oxygen species. However, at the given therapeutic doses these oxygen radicals are completely removed by antioxidants in the blood.2 Thus side effects are seen only in cases with overdose or a compromised antioxidant system.2
In our case, the wound was infected; however, we did not remove the implants in the first debridement to avoid further soft tissue damage and destabilization of the fixation. Within 5 days the wound was red, granulating with no active discharge and we did a split thickness skin graft to provide for biological dressing of the exposed bone.
With further sitting of ozone therapy and further healing of the wound we were able to perform implant removal and place a latissimus dorsi pedicle flap to cover the wound. The rapidity of infection clearance prompted us to perform the intramedullary nailing at the same time, thus achieving immediate stability and avoiding a second-stage surgery.
The patient had undergone wound debridement and intravenous antibiotics for 15 days, but rapid clearance of the infection and early granulation resulted only after ozone therapy; both local and intravenous were added to the regimen. Postoperatively, there was no relapse of infection, and healing of both soft tissue and osseous tissue was achieved without further intervention. There was no complication associated with ozone therapy.
At 20 months, the patient started leading an independent life with minimal discomfort as against the amputation offered to her. The results in our experience will help in planning further investigation in the use of ozone therapy as an adjuvant to the conventional modality for treatment of extensive orthopedic wounds.
________________________________________ |
Acknowledgements
The authors will like to acknowledge Indian Orthopaedic Research Group for help in manuscript preparation.
________________________________________ |
Footnotes
Sources of Support - Nil
Conflict of Interest: None
________________________________________ |
References
1. Bocci V. Ozone as a bioregulator.Pharmacology and toxicology of ozonetherapy today. J Biol Regul Homeost Agents. 1996;10:31–53. [PubMed]
2. Bocci V. Biological and clinical effects of ozone.Has ozone therapy a future in medicine? Br J Biomed Sci. 1999;56:270–9. [PubMed]
3. Bocci V. The clinical application of ozone therapy. In: Ozone BA, editor. A New Medical Drug.Netherlands: Springer; 2005. pp. 97–226.
4. Nogales CG, Ferrari PH, Kantorovich EO, Lage-Marques JL. Ozone therapy in medicine and dentistry. J Contemp Dent Pract. 2008;9:75–84. [PubMed]
5. Huth KC, Quirling M, Maier S, Kamereck K, Alkhayer M, Paschos E, et al. Effectiveness of ozone against endodontopathogenic microorganisms in a root canal biofilm model. Int Endod J.2009;42:3–13. [PubMed]
6. Lynch E. Evidence-based efficacy of ozone for root canal irrigation. J Esthet Restor Dent.2008;20:287–93. [PubMed]
7. Calderon NA, Kaufman T. The Microclimate Chamber: Topical Treatment of Long-Enduring Leg Ulcers with Ozone. 3rd International Symposia on Ozone Applications. 2000
8. de Monte A, van der Zee H, Bocci V. Major ozonated autohemotherapy in chronic limb ischemia with ulcerations. J Altern Complement Med. 2005;11:363–7. [PubMed]
9. Bocci VA. Why orthodox medicine has not yet taken advantage of ozone therapy. Arch Med Res.2008;39:259–60. [PubMed]
10. Azarpazhooh A, Limeback H. The application of ozone in dentistry: a systematic review of literature. J Dent. 2008;36:104–16. [PubMed]
11. Bocci V, Di Paolo N. Oxygen-ozone therapy in medicine: an update. Blood Purif. 2009;28:373–6.[PubMed]
12. Roth E, Jancsó G. Pathology and diagnostic options of lower limb compartment syndrome. Clin Hemorheol Microcirc. 2009;41:1–8. [PubMed]
13. Re L, Mawsouf MN, Menéndez S, León OS, Sánchez GM, Hernández F. Ozone therapy: clinical and basic evidence of its therapeutic potential. Arch Med Res. 2008;39:17–26. [PubMed]
14. Bocci VA. Scientific and medical aspects of ozone therapy.State of the art. Arch Med Res.2006;37:425–35. [PubMed]
15. Valacchi G, Bocci V. Studies on the biological effects of ozone: 11.Release of factors from human endothelial cells. Mediators Inflamm. 2000;9:271–6. [PMC free article] [PubMed]
16. Valacchi G, Bocci V. Studies on the biological effects of ozone: 10.Release of factors from ozonated human platelets. Mediators Inflamm. 1999;8:205–9. [PMC free article] [PubMed]
17. Giunta R, Coppola A, Luongo C, Sammartino A, Guastafierro S, Grassia A, et al. Ozonized autohemotransfusion improves hemorheological parameters and oxygen delivery to tissues in patients with peripheral occlusive arterial disease. Ann Hematol. 2001;80:745–8. [PubMed]
18. Bocci V, Aldinucci C, Mosci F, Carraro F, Valacchi G. Ozonation of human blood induces a remarkable upregulation of heme oxygenase-1 and heat stress protein-70. Mediators Inflamm.2007;2007:26785. [PMC free article] [PubMed]
19. Zuckerbraun BS, Billiar TR. Heme oxygenase-1: a cellular Hercules. Hepatology. 2003;37:742–4.[PubMed]
20. Bocci V, Borrelli E, Travagli V, Zanardi I. The ozone paradox: ozone is a strong oxidant as well as a medical drug. Med Res Rev. 2009;29:646–82. [PubMed]
21. Dorshkind K, Swain S. Age-associated declines in immune system development and function: causes, consequences, and reversal. Curr Opin Immunol. 2009;21:404–7. [PMC free article][PubMed]
22. Bocci V. The case for oxygen–ozone therapy. Br J Biomed Sci. 2007;64:44–9. [PubMed]
23. Bocci V, Luzzi E, Corradeschi F, Paulesu L. Studies on the biological effects of ozone: 5. Evaluation of immunological parameters and tolerability in normal volunteers receiving ambulatory autohaemotherapy. Biotherapy. 1993;7:83–90. [PubMed]
24. Seidler V, Linetskiy I, Hubálková H, Stanková H, Smucler R, Mazánek J. Ozone and its usage in general medicine and dentistry.A review article. Prague Med Rep. 2008;109:5–13.
________________________________________ |
Medical Science News - Information Scientific Medicale
Journal List > Indian J Orthop > v.45(4); Jul-Aug 2011
Indian J Orthop. 2011 Jul-Aug; 45(4): 376–379. doi: 10.4103/0019-5413.8033
By: Dr. Prasham Shah, Ashok K Shyam, and Sambhav Shah
E-mail: drashokshyam@yahoo.co.uk
Ref: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3134027/
|